SHPBN-2015-037 Claims Submission for Coordination of Benefits (COB) & Third Party Liability (TPL)
Date: 09/23/15
(HCBS providers, see SHPBN-2016-045 for additional information.)
Submission of COB and TPL Claims
If probable existence of other insurance is established at the time a claim is filed, Sunflower Health Plan will deny the claim and the provider will be required to bill the primary carrier before resubmitting the claim. This means that the provider must attempt to bill the other insurance company prior to filing the claim to Sunflower Health Plan.
COB / TPL Claim Submission Requirements
Tertiary Coverage
Tertiary coverage must be billed on a paper claim. Tertiary coverage cannot be processed on the Secure Provider Web Portal or electronically through a clearinghouse.
COB / TPL Paper Claim Submissions
(reference Sunflower Provider Office Manual)
CMS-1500
- Complete one of the following to indicate other insurance is involved:
- Fields 9 and 9A-D (Other Insured’s Name)
- Field 11 and 11A-D (Insured’s Policy Group or FECA Number)
- Field 29 (Amount Paid) – Make sure it is completed with any amount paid by insurance or other third party sources known at the time the claim is submitted. If the amount shown in this field is the result of other insurance, documentation of the payment must be attached. Do not enter copayment or spenddown payment amounts. They are deducted automatically.
- Providers submitting claims electronically must include TPL/COB information for each detail line level, where applicable.
UB-04
- Field 50 (Payer Name) - Indicate all third party resources (TPR). If TPR exists, it must be billed first.
- Lines B and C should indicate secondary and tertiary coverage. Medicaid will be either the secondary or tertiary coverage and the last payer. When B and C are completed, the remainder of this line must be completed as well as Fields 58-62.
- Field 54 (Prior Payments Payer) – Required if other insurance is involved. Enter amount paid by other insurance. Documentation of the payment must be attached. Do not enter copayment or spenddown payment amounts. They are deducted automatically.
- Field 58 (Insured’s Name) – Required.
- Field 59 (Patient’s Relationship to Insured)
- Line A – Required.
- Line B and C – Situational.
- Field 60 (Insured’s Unique ID) – Required. Enter the 11-digit beneficiary number from the State of Kansas Medicaid Card on Line C. If billing for newborn services, use the mother's beneficiary number. The mother's number should only be used if the newborn's ID number is unknown.
- Field 61 (Insured’s Group Name) – Required, if group name is available. Enter the primary insurance information on Line A and Medicare on Line C.
- Field 62 (Insured’s Group Number) – Required, when insured’s ID card shows a group number.
Submit first-time paper claims and claim reconsiderations with the other insurance coverage EOP(s) directly to Sunflower Health Plan to P.O. Box 4070, Farmington, MO, 63640-3833.
COB / TPL Electronic Claim Submissions
(reference Sunflower Provider Office Manual)
Sunflower has the ability to receive coordination of benefit (COB or Secondary) claims electronically.
The field requirements for successful electronic COB submission are below (5010 Format):
COB Field Name The below should come from the primary payer's Explanation of Payment | 837I - Institutional EDI Segment and Loop | 837P - Professional EDI Segment and Loop COB INFORMATION MUST BE SUBMITTED AT DETAIL LINE LEVEL |
|---|---|---|
COB Paid Amount | If 2320/AMT01=D, MAP AMT02 or 2430/SVD02 | If 2320/AMT01=D, MAP AMT02 or 2430/SVD02 |
COB Total Non-Covered Amount | If 2320/AMT01=A8, map AMT02 | If 2320/AMT01=A8, map AMT02 |
COB Remaining Patient Liability | If 2300/CAS01 = PR, map CAS03 Note: Segment can have 6 occurrences. Loop2320/AMT01=EAF, map AMT02 which is the sum of all of CAS03 with CAS01 segments presented with a PR | If 2320/AMT01=EAF, map AMT02 |
COB Patient Paid Amount |
| If 2320/AMT01 = F5, map AMT02 |
COB Patient Paid Amount Estimated | If 2300/AMT01=F3, map AMT02 |
|
Total Claim Before Taxes Amount | If 2400/AMT01 = N8, map AMT02 | If 2320/AMT01 = T, map AMT02 |
COB Claim Adjudication Date | IF 2330B/DTP01 = 573, map DTP03 | IF 2330B/DTP01 = 573, map DTP03 |
COB Claim Adjustment Indicator | IF 2330B/REF01 = T4, map REF02 | IF 2330B/REF01 = T4, map REF02 with a Y |
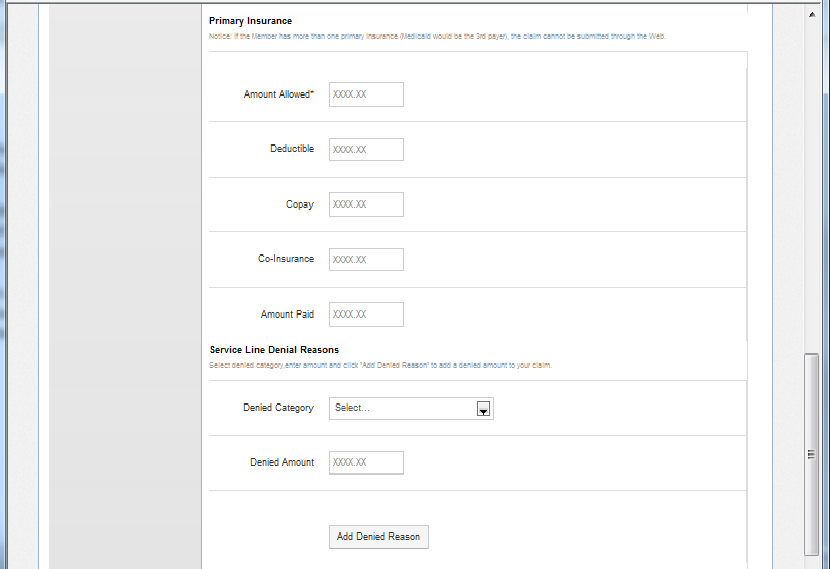
COB / TPL Web Portal Claim Submission
Providers who have created a login account for the Secure Web Portal may use it to submit COB / TPL Claims. A Secure Provider Website Manual is available for reference, once you have logged in. Reference the 'Coordination of Benefits' section for general instruction on the submission of secondary claims. As a gentle reminder, Tertiary claims may not be submitted using the Secure Web Portal and must be submitted on paper, as described above.
When using the Secure Web Portal to indicate the primary payer does not cover a service:
- Populate the other insurance fields with all zeroes, or ‘X’.
- For professional claims, this field should be populated each line item billed.
By populating the other insurance fields with ‘X’ (as provided in the example screen below), the provider’s TPL Information will be captured by the claims system for coordination of benefit (COB). This will allow Sunflower to process the claim. All documentation from the third party payor indicating a denial for service must be kept on file with the provider.
Please contact your Provider Relations Representative if you are interested in scheduling training on the use of Sunflower Health Plan's Secure Provider Web Portal. To identify the Provider Relations Representative for your area, reference our Sunflower Provider Relations Territory Map.
If you have questions, please call Customer Service at 1-877-644-4623.

